The Future: Telehealth and Home Care

The Issue
Out of every crisis, a new opportunity arises. For telehealth and home care, COVID-19 may herald an opportunity whose time has finally come. While the volumes of telehealth consults in Canada and the United States have gone up several multiples since the pandemic struck, there are decidedly different perspectives among hospital and health-care planners about whether telehealth is a short-lived bubble or the wave of the future.
The salient questions raised are three: How broad has been utilization of these services, pre- and post COVID-19? Can this increased demand enhance health care treatment and outcomes? What are the prospects for these enhancements becoming an ongoing significant part of the future of our health care?
Ethical and Moral Challenges
Telemedicine is not new. For millennia, the laying-on of hands represented the essence of the doctor-patient relationship: taking the pulse, tapping on and listening to the chest, feeling lumps—the human touch of the care-giver. But the COVID-19 pandemic is accelerating the transition to a new model of remotely delivered health care that embraces the benefits of digital and data technologies. It is not a solution to the current pandemic, but it will be one of lasting consequences.
Prior to COVID-19, telehealth captured a small part of total health care. It is practiced globally in only a handful of countries. Canada was an early pioneer in the development of virtual care through the work of the late Dr. Maxwell House of Memorial University of Newfoundland in the 1970s; he used telephone technology to provide virtual consultations to remote sites throughout the province. Canada has since been surpassed by other countries in the uptake of virtual care.
Estimates of penetration as a percentage of general practice appointments in Canada, England and the US respectively are 8, 14, and 10-18 per cent. Some US systems have been using telehealth routinely for years, and employers—especially larger employers—have been adding it to coverage at a rapid clip, using it to increase worker convenience and to cut costs. In recent years, telehealth has gradually come into use in obstetrics care, typically in rural areas but also in some urban areas where some pregnant women, such as certain immigrants, may be less inclined or able to visit medical facilities.
There are various reasons for and indicators that demand for telemedicine, (variously called virtual care, remote care, home care, distance health, remote-delivery medicine, hospital at home, or more properly telehealth), has been surging during the past two months :
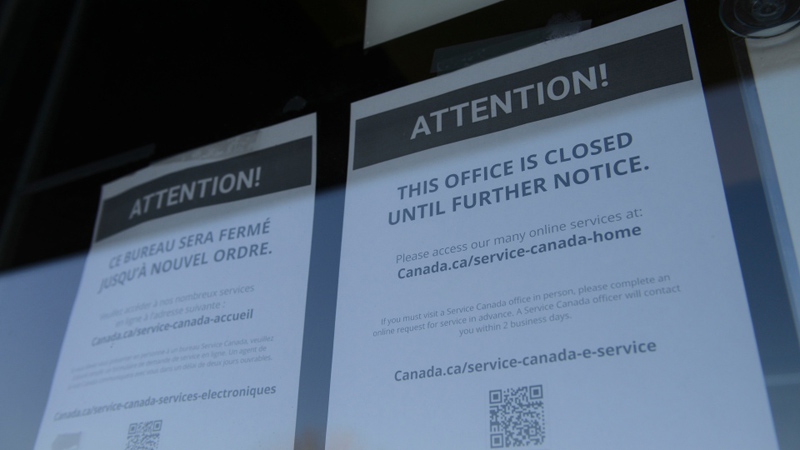
- Many physicians have closed their offices and resorted to referring their patients to government-funded telehealth services.
- Front-line health-care workers have been swamped since the coronavirus outbreak by the number of calls.
- Many health systems are turning to self-triaging tools to help consumers check for symptoms before asking to be put through to a doctor.
- COVID-19 has resulted in a surge of demand for reassurance and personal attention from their trusted health care provider, including patients who want to speak with their physicians about possible symptoms and treatment for COVID-19.
- Virtual visits to chatbots or doctor-free screening in certain cities like Vancouver and Seattle are occurring 10-15 times more than pre-pandemic levels.
Critics argue that telehealth has not had the success story it had hoped to achieve. The method, involving remote health-related services such as monitoring, advice and education between doctors and patients online over a secure connection, promised to be at the forefront of the future of medicine. It was touted as being able to make state-of-the-art health care more accessible and affordable without the need to wait hours in line.
While telemedicine has been steadily on the rise for years, with companies around the world helping patients, it has not become a mainstream or universal form of patient interaction for various reasons:
- (a) It defies the time-honoured custom (and remuneration associated with) a physical visit.
- (b) It needs to overcome regulatory and commercial hurdles, including requiring a digital infrastructure that ensures secure connections between patients and physicians.
- (c) Many physicians are self- employed professionals who remain resistant to alternative or third party forms of delivery of their services.
- (d) The traditional ambulance-hospital-convalescent home model is well entrenched and resistant to change.
As people worldwide face a COVID lockdown there is a greater need for testing, nursing care and medical consultations. Thus, remote health care is an important part of the response, hastening the telemedicine trend that has already been under way. Much of the technology already exists, and more is quickly being developed to combat the novel coronavirus.

In some jurisdictions, patients and their family members report high levels of satisfaction with at-home care. Internationally, hospital-at-home programs have been piloted successfully in countries including Australia, Canada, Italy, New Zealand and the United Kingdom. In one meta-analysis, home-based hospital care in these countries was shown to be safe and reduce mortality in the six months after patients received hospital-level care, while also reducing costs.
As of 2019, the telemedicine global market was valued at some 45 billion U.S. dollars. Its widest current applications are in dermatology, psychiatry, intensive care units, emergency care, ophthalmology, and radiology, out of which, tele-radiology accounted for the majority of revenue in 2019. The market is expected to grow significantly by 2026 to be valued at more than 175 billion U.S. dollars at that time.
Legal and Values Opportunities and Challenges

Combing various infectious disease diagnosis and treatment studies reveals that major benefits of telehealth at this time of coronavirus include:
- (a) Virtual visits yield professional advice without compromising the health of physicians or patients. Patients can have a rapid “video visit” with a doctor or a nurse and avoid going to a clinic teeming with other people who are possibly infected. And they won’t be a risk to the medical professionals who might otherwise be exposed.
- (b) Telehealth platforms enable patient families to speak with their loved ones in acute care.
- (c) Hospital-at-home programs can reduce health-care costs and mortality rates, including easing pressure on hospitals and allowing more patients to be seen in a shorter time.
- (d) During the pandemic, providing hospital care at home can reduce the risk of COVID-19 transmission, especially for vulnerable patients.
- (e) Telehealth frees up staff to treat patients while following safe distancing rules.
- (f) The practice enhances necessary remote patient monitoring (RPM), home testing kits, and home monitoring. While RPM has grown steadily in the past couple of years, current shelter-at-home restrictions across the country have highlighted the need to monitor patients with chronic conditions in their homes.
- (g) Telehealth enhances tracking and testing. Patients under investigation (PUI) who are suspected of having been infected with COVID-19 can be monitored closely, as are others who are worried about their risks (the “worried well”).
- (h) Resilient, versatile companies and public health agencies can find it easier to apply the lessons learned from the present crisis to find ways to repurpose existing assets in preparation for the next crisis. For example:
- (i) hotels are turning into makeshift hospitals;
- (ii) sport and concert arenas are turning into logistics hubs, and
- (iii) robotic s can be used to monitor patients, deliver supplies, and disinfect wards.
- (i) Telehealth reduces travel carbon emissions and addresses climate change and sustainability challenges.
- (j) Home care programmes are feasible, save resources and prevent in-hospital transmission of COVID-19.
One of the problematic elements of assessing the prospects for telehealth is that the same advantage can also serve as a disadvantage. The system is a closed loop. For example, telehealth successes in identifying infected carriers can actually then potentially over-load hospital systems. Likewise treatment successes with providing at-home monitoring, counselling and obstetrics care can threaten the current business model of ambulance to hospital to convalescent home care.

While most health systems seem to have successfully scaled up their telehealth operations, some have seen a rise in wait times that have negated the premise of “on-demand” or “home-based” care through virtual health tools. A summary of telehealth’s problems or COVID limitations includes:
- Patients who get triaged for COVID-19 screening have had to wait in a virtual queue because of the sudden spike in the number of virtual visits. The lack of available trained clinicians to take on virtual consults has exacerbated the problem.
- Deploying same-day, express care clinician to follow up, and attend to the needs of newly triaged patients coming in through the chatbots is a challenge.
- As we climb out of the pandemic, traditional health systems will streamline their processes and bring more clinicians on board, which will help flatten out the learning curve as well.
- Silicon Valley Big Tech firms, always quick to respond with technology to marketplace needs, have seen a lukewarm response to new tracking and tracing tools offered by start-ups and Big Tech firms.
- Google parent Verily’s symptom triaging tool for COVID-19 has come under criticism from privacy advocates, highlighting privacy concerns and the lack of trust that epitomizes the challenges for digital-health companies in general.
The Future
Professionals hold flatly contradictory assessments and forecasts about telehealth’s accomplishments in treating COVID-19, including its success, its limitations, and its cultural limitations. EthicScan is offering a learning circle including a staged program of scenario development and testing to assess its future compared to that of primary care, hospital care, long-term care facilities, and other alternatives.
Even if we cannot forecast the immediate duration, possible transformation and future of COVID-19, it is not unreasonable that another global public-health crisis is likely to happen. In less than a decade we’ve seen the likes of MERS, Ebola, Zika virus and COVID-19. The current, latest one has shown the importance of conducting strategic analyses on benefitting from telehealth. Key stakeholders should embrace the benefits of this digital technology in our new digital economy, while also preparing for an eventual emergency.
Further Reading
CIO – How the COVID-19 pandemic is reshaping healthcare with technology:
https://www.cio.com/article/3534499/how-the-covid-19-pandemic-is-reshaping-healthcare-with-technology.html
World Economic Forum – Why we should expand hospital-at-home during the COVID-19 pandemic:
https://www.weforum.org/agenda/2020/04/hospital-at-home-covid19-coronavirus-pandemic-nursing-care/
The Globe and Mail – Will Virtual Healthcare be the New Normal after COVID-19?
https://www.theglobeandmail.com/life/health-and-fitness/article-will-virtual-healthcare-be-the-new-normal-after-covid-19/
Healthcare IT News – COVID-19: How the coronavirus crisis will change the care model:
https://www.healthcareitnews.com/news/europe/covid-19-how-coronavirus-crisis-will-change-care-model
The Economist – Telemedicine is essential amid the covid-19 crisis and after it:
https://www.economist.com/open-future/2020/03/31/telemedicine-is-essential-amid-the-covid-19-crisis-and-after-it
The Medical Futurist – COVID-19 and the rise of Telemedicin:
https://medicalfuturist.com/covid-19-was-needed-for-telemedicine-to-finally-go-mainstream/
Health Leaders Media – NCHA President Steve Lawler on COVID-19 and the Future of Telehealth:
https://www.healthleadersmedia.com/finance/ncha-president-steve-lawler-covid-19-and-future-telehealth
World Health Organization – https://apps.who.int/iris/rest/bitstreams/1272288/retrieve
Medical Futurist:COVID-19 was needed for telemedicine to finally go mainstream:
https://medicalfuturist.com/covid-19-was-needed-for-telemedicine-to-finally-go-mainstream/
- Radically Remaking the Future of Transit Industry Post COVID - November 16, 2020
- Radically Remaking the Future of Retailing Industry Post COVID - November 12, 2020
- Radically Remaking the Future of Restaurant Industry Post-COVID - November 12, 2020
